Blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term “blood pressure” refers to the pressure in the large arteries. Blood pressure is usually expressed in terms of systolic pressure (maximum pressure during one heartbeat) over diastolic pressure (minimum pressure between two heartbeats) in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure.
Healthy and unhealthy blood pressure ranges
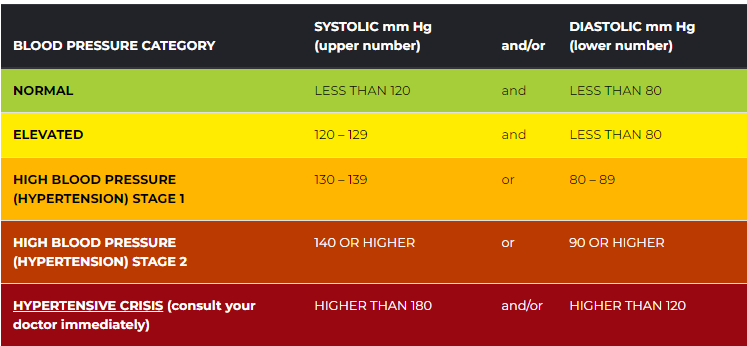
Blood pressure categories
The five blood pressure ranges as recognized by the American Heart Association are:
- Normal
Blood pressure numbers of less than 120/80 mm Hg are considered within the normal range. If your results fall into this category, stick with heart-healthy habits like following a balanced diet and getting regular exercise. - Elevated
Elevated blood pressure is when readings consistently range from 120-129 systolic and less than 80 mm Hg diastolic. People with elevated blood pressure are likely to develop high blood pressure unless steps are taken to control the condition. - Hypertension Stage 1
Hypertension Stage 1 is when blood pressure consistently ranges from 130-139 systolic or 80-89 mm Hg diastolic. At this stage of high blood pressure, doctors are likely to prescribe lifestyle changes and may consider adding blood pressure medication based on your risk of atherosclerotic cardiovascular diseases (ASCVD), such as heart attack or stroke. - Hypertension Stage 2
Hypertension Stage 2 is when blood pressure consistently ranges at 140/90 mm Hg or higher. At this stage of high blood pressure, doctors are likely to prescribe a combination of blood pressure medications and lifestyle changes. - Hypertensive crisis
This stage of high blood pressure requires medical attention. If your blood pressure readings suddenly exceed 180/120 mm Hg, wait five minutes and then test your blood pressure again. If your readings are still unusually high, contact your doctor immediately. You could be experiencing a hypertensive crisis.
Disorders of blood pressure
High blood pressure. Hypertension
Overview of main complications of persistent high blood pressure
Arterial hypertension can be an indicator of other problems and may have long-term adverse effects. Sometimes it can be an acute problem, for example, hypertensive emergency.
Levels of arterial pressure put mechanical stress on the arterial walls. Higher pressures increase heart workload and progression of unhealthy tissue growth (atheroma) that develops within the walls of arteries. The higher the pressure, the more stress that is present and the more atheroma tends to progress and the heart muscle tends to thicken, enlarge and become weaker over time.
Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure, and arterial aneurysms, and is the leading cause of chronic kidney failure. Even moderate elevation of arterial pressure leads to shortened life expectancy. At severely high pressures, mean arterial pressures 50% or more above average, a person can expect to live no more than a few years unless appropriately treated.
In the past, most attention was paid to diastolic pressure; but nowadays it is recognized that both high systolic pressure and high pulse pressure (the numerical difference between systolic and diastolic pressures) are also risk factors. In some cases, it appears that a decrease in excessive diastolic pressure can actually increase risk, due probably to the increased difference between systolic and diastolic pressures (see Pulse pressure). If systolic blood pressure is elevated (>140 mmHg) with normal diastolic blood pressure (<90 mmHg), it is called “isolated systolic hypertension” and may present a health concern.
For those with heart valve regurgitation, a change in its severity may be associated with a change in diastolic pressure. In a study of people with heart valve regurgitation that compared measurements two weeks apart for each person, there was an increased severity of aortic and mitral regurgitation when diastolic blood pressure increased, whereas when diastolic blood pressure decreased, there was a decreased severity.
Low blood pressure. Hypotension
Blood pressure that is too low is known as hypotension. This is a medical concern if it causes signs or symptoms, such as dizziness, fainting, or in extreme cases, circulatory shock.
Causes of low arterial pressure include:
- Sepsis
- Hemorrhage – blood loss
- Cardiogenic shock
- Neurally mediated hypotension (or reflex syncope)
- Toxins including toxic doses of blood pressure medicine
- Hormonal abnormalities, such as Addison’s disease
- Eating disorders, particularly anorexia nervosa and bulimia
Orthostatic hypotension. Orthostatic hypotension
A large fall in blood pressure upon standing (persistent systolic/diastolic blood pressure decrease of >20/10 mm Hg) is termed orthostatic hypotension (postural hypotension) and represents a failure of the body to compensate for the effect of gravity on the circulation. Standing results in increased hydrostatic pressure in the blood vessels of the lower limbs. The consequent distension of the veins below the diaphragm (venous pooling) causes ~500 ml of blood to be relocated from the chest and upper body. This results in a rapid decrease in central blood volume and a reduction of ventricular preload which in turn reduces stroke volume, and mean arterial pressure. Normally this is compensated for by multiple mechanisms, including activation of the autonomic nervous system which increases heart rate, myocardial contractility, and systemic arterial vasoconstriction to preserve blood pressure and elicits venous vasoconstriction to decrease venous compliance. Decreased venous compliance also results from an intrinsic myogenic increase in venous smooth muscle tone in response to the elevated pressure in the veins of the lower body. Other compensatory mechanisms include the veno-arteriolar axon reflex, the ‘skeletal muscle pump’, and the ‘respiratory pump’. Together these mechanisms normally stabilize blood pressure within a minute or less. If these compensatory mechanisms fail and arterial pressure and blood flow decrease beyond a certain point, the perfusion of the brain becomes critically compromised (i.e., the blood supply is not sufficient), causing lightheadedness, dizziness, weakness, or fainting. Usually, this failure of compensation is due to disease, or drugs that affect the sympathetic nervous system. A similar effect is observed following the experience of excessive gravitational forces (G-loading), such as routinely experienced by aerobatic or combat pilots ‘pulling Gs’ where the extreme hydrostatic pressures exceed the ability of the body’s compensatory mechanisms.
Variable or fluctuating blood pressure
Some fluctuation or variation in blood pressure is normal. Variations in pressure that are significantly greater than the norm are associated with increased risk of cardiovascular disease brain small vessel disease, and dementia independent of the average blood pressure level. Recent evidence from clinical trials has also linked variation in blood pressure to mortality, stroke, heart failure, and cardiac changes that may give rise to heart failure. These data have prompted discussion of whether excessive variation in blood pressure should be treated, even among normotensive older adults. Older individuals and those who had received blood pressure medications are more likely to exhibit larger fluctuations in pressure, and there is some evidence that different antihypertensive agents have different effects on blood pressure variability; whether these differences translate to benefits in outcome is uncertain.
sources : heart.org; Wikipedia
- Pfizer voluntarily recalls some lots of blood pressure drug due to potential carcinogen
- Pfizer pulls blood pressure med in Canada on carcinogen fears



OF NATURAL PRODUCTS AND EXTRACTS


